Your Audiology Tutorial: Headshake Nystagmus
The observation for what is known as headshake nystagmus is sometimes part of a vestibular work up to determine the ear-related cause of a patient's dizziness. The clinician is checking, via the direction of the patient's eye movement, if one of the semicircular canal labyrinths has a lesion. This is a test of peripheral vestibular function, but those with central dysfunction may also be identified, again based on how the eyes are moving post test.
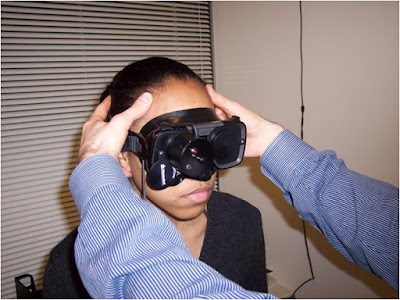
The patient is asked to tilt head forward about thirty degrees and shake head quickly in the horizontal plane for twenty to thirty seconds. The test may also be repeated in the vertical plane, with patient nodding their head for the same amount of time. The examiner, who can either directly observe patient or have them wear a mask with Frenzel lenses with recording capabilities, may assist with this process.
The patient is asked to tilt head forward about thirty degrees and shake head quickly in the horizontal plane for twenty to thirty seconds. The test may also be repeated in the vertical plane, with patient nodding their head for the same amount of time. The examiner, who can either directly observe patient or have them wear a mask with Frenzel lenses with recording capabilities, may assist with this process.
Afterward, the pupils and irises are examined for movement (nystagmus) in a horizontal path. The ear which the eyes are moving (beating) away from may indicate the more neurologically active side, the site of lesion. This test is arguably useful in correlation with the air/water caloric test performed during the VNG battery. Post headshake nystagmus has been shown to be more prevalent in patients with a unilateral vestibular weakness.
Comments